A simple blood draw can provide physicians with valuable information that can determine if peptide receptor radionuclide therapy (PRRT) is likely to be effective in a patient with neuroendocrine cancer. The blood-based biomarker PPQ can predict which patients will respond to PRRT with 96 percent accuracy; changes in another biomarker, NETest, correctly correlate with PRRT response in 90 percent of patients. The study, published in the April issue of The Journal of Nuclear Medicine, opens new possibilities of tailoring radiopharmaceutical treatment to patients.
While biomarkers have been used to predict the outcomes of treatments for breast, prostate, and other cancers, there are currently no objective means to predict the efficacy of radiopharmaceutical therapy for neuroendocrine tumors. “In previous studies our team introduced the blood-based biomarkers PPQ and NETest as a measure for determining whether treatment with PRRT would be successful,” noted Lisa Bodei, MD, PhD, nuclear medicine physician at Memorial Sloan Kettering Cancer Center in New York, New York. “In this new study we sought to validate the role of PPQ and NETest in predicting response and monitoring PRRT.”
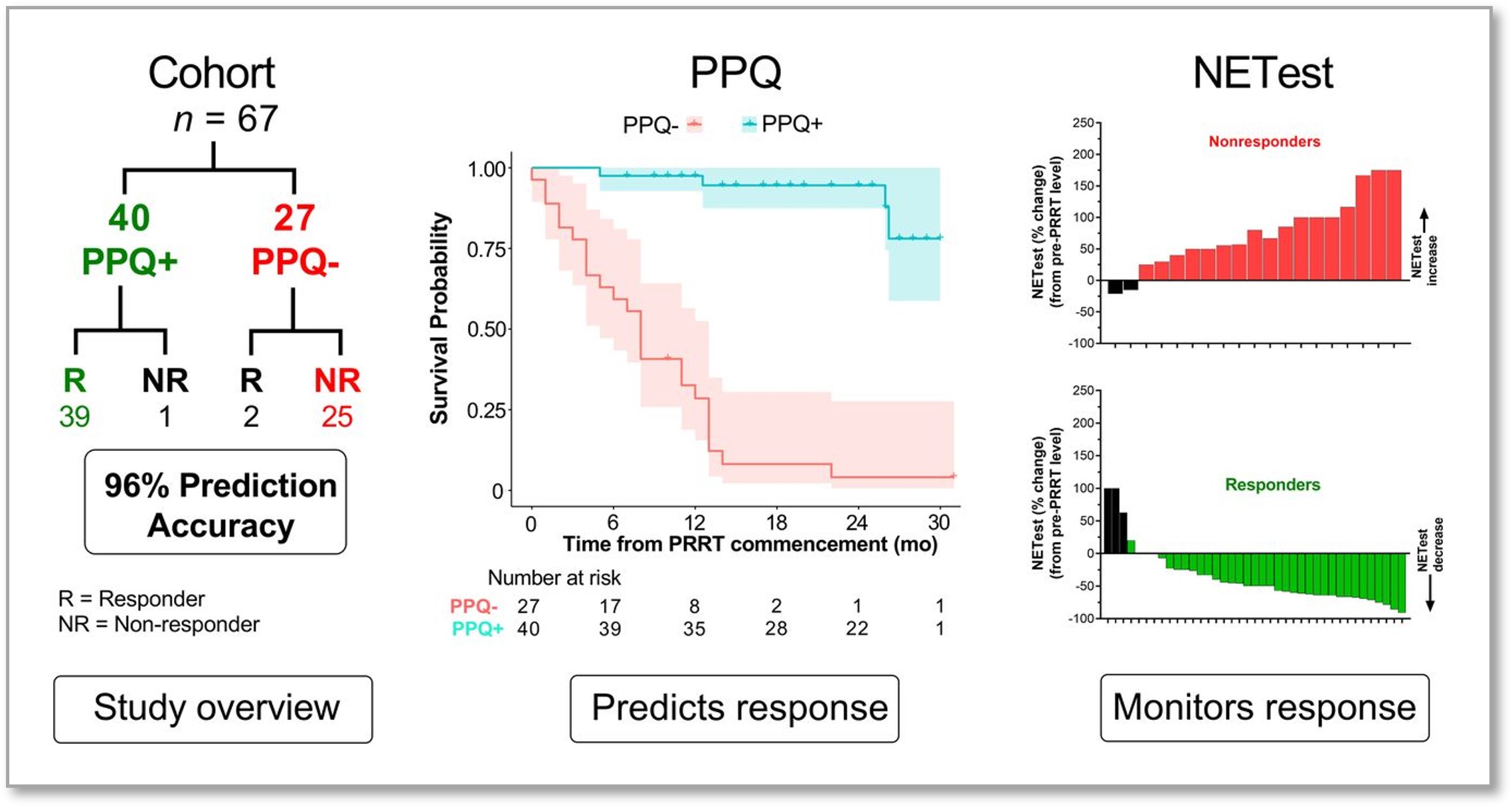
Sixty-seven patients with somatostatin receptor-positive gastroenteropancreatic and lung neuroendocrine tumors were included in the study. All patients had metastatic disease and had received prior treatments. Blood samples were collected before each cycle of PRRT and at follow-up. PPQ was scored as either positive (likely to respond) or negative (unlikely to respond), and NETest was measured on a scale of zero to 100, with the upper limit of normality being 20.
Of the 67 patients in the study, 40 were classified as PPQ+, and 39 of them (98 percent) responded to PRRT. Twenty-seven patients were PPQ–, and 25 patients in this group experienced disease progression despite PRRT. The overall predictive accuracy of PPQ was 96 percent.
NETest was elevated in all patients prior to PRRT therapy. For PRRT responders, baseline NETest levels were 67, which decreased by 37 percent after treatment. For non-responders, baseline NETest levels were 44, which increased by 76 percent at follow-up. The NETest biomarker was 90 percent accurate for determining PRRT response.
“The results of this study demonstrate that not all tumors are created equal; some are more prone to respond to PRRT, and some are less susceptible to radiopharmaceutical therapy,” said Bodei. “This is the reason why our research is important: to understand from the start which patients will require an intensified treatment plan and which patients, instead, can benefit from a lighter regimen will tremendously improve their management.”