PET/CT imaging with F-18 fluorodopa (FDOPA) is an effective approach for detecting neuroendocrine tumors (NETs) -- and now the scans may be used to predict survival in patients with tumors in the midgut, according to researchers in France.
A team at Beaujon Hospital in Clichy found that patients with high tumor uptake of FDOPA radiotracer on PET/CT had significantly shorter survival. This is key information for clinicians as they develop strategies to improve outcomes for patients, the group noted. The findings were published August 31 in the Journal of Nuclear Medicine.
"We demonstrated that F-18 FDOPA-PET/CT has a significant prognostic impact in patients with metastatic midgut NETs," wrote first author Ophélie De Rycke, MD, and colleagues.
Cases of NETs -- a heterogeneous group of rare neoplasms -- are increasing, with the midgut among the most frequent locations, the authors explained. F-18 FDOPA-PET/CT reveals these tumors based on visualizing higher than normal metabolism of 3,4-dihydroxyphenylalanine (DOPA) by NET cells. The approach has excellent performance for helping to diagnose these tumors and is used routinely at their hospital, the authors wrote.
"Whereas the diagnostic role of F-18 FDOPA-PET/CT is now well described, its prognostic impact has never, to our knowledge, been explored," the group wrote.
To that end, the researchers gathered imaging from 252 patients with midgut NETs and liver metastases who underwent at least one whole-body F-18 FDOPA-PET/CT scan between January 2010 and January 2021 in one of five French centers. They split the group into a test cohort (n = 166) and then sought to validate the results in a group of 86 patients.
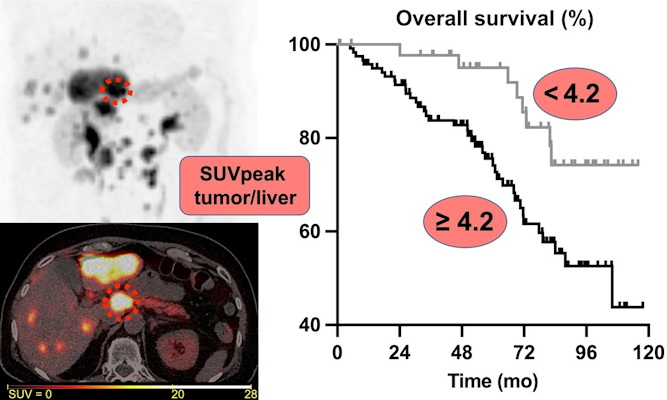
A visual abstract. Image courtesy of the Journal of Nuclear Medicine.
All scans were reviewed at each site by an expert nuclear medicine physician masked to the clinical and survival data. The primary endpoint was overall survival, measured between the date of the first F-18 FDOPA- PET/CT scan and the date of death from any cause.
According to the analysis, patients with F-18 FDOPA tumor-to-liver (T/L) ratio on PET/CT of more than 4.2 had significantly shorter survival than those with a ratio of 4.2 or less (p = 0.01) -- a five-year overall survival rate of 74.1% versus 95%. Moreover, based on the same values, the five-year survival rate was 100% versus 57.8% in the validation cohort.
"An increasing SUVpeak T/L ratio over time tended to have a pejorative prognostic impact," the group wrote.
Ultimately, the study suggests that tumor uptake measured on F-18 FDOPA-PET/CT could contribute to a better assessment of the prognosis of patients with metastatic midgut NETs and may be a better choice for patient management, the authors wrote.
They noted, however, that the mechanisms underlying the prognostic impact of F-18 FDOPA PET/CT are unclear and that additional molecular studies could lead to potential targets for new therapies.
"Future translational studies should explore the molecular bases of this prognostic impact and aim at identifying potential related therapeutic targets," the group concluded.