Combining PET/CT with traditional clinical risk factors can detect prostate cancer in cases considered borderline based on prostate-specific antigen (PSA) levels -- in other words, cases in the "PSA grey zone," according to a group in Hunan, China.
Ultimately, the approach could reduce the need for invasive biopsy procedures to confirm a diagnosis, suggested a team led by Jinhui Yang, MD, of Central South University's Xiangya Hospital.
"There is an urgent need for a highly accurate and noninvasive alternative for the early diagnosis of [prostate cancer] and to reduce unnecessary biopsies, especially for patients who fall within the PSA gray zone," the group wrote, in a study published September 4 in Cancer Imaging.
Prostate cancer is the second most common cancer and the fifth leading cause of cancer death among men around the world, with PSA tests widely used to diagnose the disease, the authors noted. Yet PSA levels between 4-10 nanograms per milliliter (ng/mL) may indicate nonmalignant conditions such as benign prostatic hyperplasia (BPH), prostatic hyperplasia, or urinary tract infections, they wrote.
Moreover, while gallium-68 (Ga-68) prostate-specific membrane antigen (PSMA) PET imaging has revolutionized diagnosis of the disease since its approval in 2020, studies have shown it also may be limited in detecting low-risk cases, they added.
Thus, in this study, the researchers aimed to develop a predictive model based on Ga-68 PSMA-PET/CT findings and additional clinical indicators to improve its performance and ultimately mitigate the need for biopsies.
The group gathered data on 81 consecutive patients who had two or more tests showing increased serum total PSA levels between 4 and 10 ng/mL from September 2019 to January 2022. Patients also underwent image-guided biopsies, and the researchers divided the patients into groups with clinically significant cases and non-clinically significant cases.
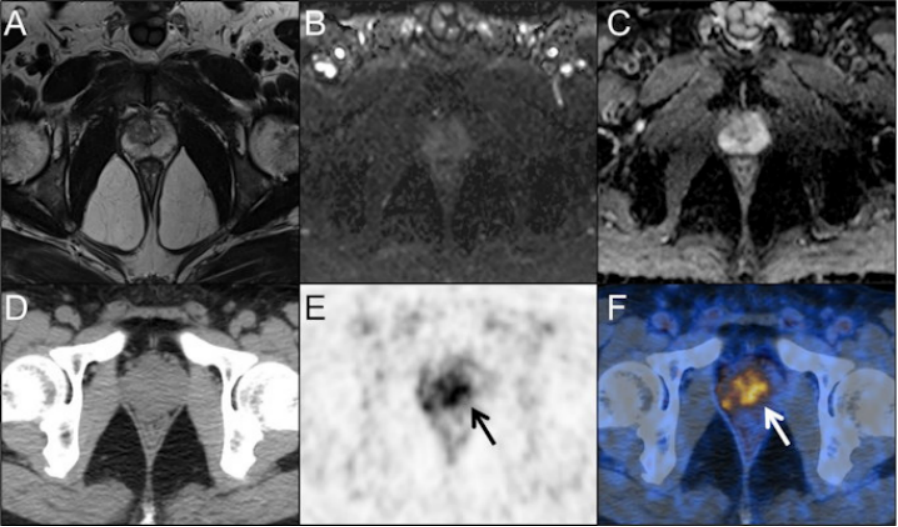
A 55-year-old man presented with a persistently elevated prostate-specific antigen (PSA) range of 4.37-6.82 ng/ml over a period of one year. Magnetic resonance imaging (MRI) (A, T2-weight imaging; B, DWI imaging; C, ADC map) didn't reveal the presence of any malignant lesions. PET/CT images (D, CT; E, PET; F, fusion) showed intensive prostate-specific membrane antigen (PSMA) uptake in the center gland and right periphery of the prostate (arrows). According to the predictive model, the probability of clinically significant prostate cancer for this lesion is 0.67 (> 0.35). Subsequent prostate biopsy result in a Gleason score 4 + 3 prostate cancer. Image courtesy of Cancer Imaging through CC BY 4.0.
In the analysis, they compared a number of diagnostic indicators between the groups. They found a prediction model comprised of Ga-68 PSMA PET/CT maximum standardized uptake value (SUVmax), prostate volume (PV), and free PSA/total PSA (a ratio indicating risk) performed best for identifying clinically significant cases.
The model achieved an area under the operating curve (AUC) of 0.927 compared with all other predictors alone, and a diagnostic sensitivity of 86% and a specificity of 87%, they found.
"Given the low diagnostic accuracy of regular PSA tests, a new prediction model based on the Ga-68 PSMA-PET/CT SUVmax, PV, and FPSA/TPSA was developed and validated, and this model could provide a more satisfactory predictive accuracy," the researchers wrote.
Ultimately, PSA alone in the gray zone is not appropriate for diagnosing clinically significant prostate cancer, the authors wrote. In challenging tumors, clinicians need new powerful biomarkers to be able to improve patient management, and by combining imaging, analytical, and clinical parameters, they can achieve this, they suggested.
"This study provides a noninvasive prediction model with high accuracy for the diagnosis of [clinically significant prostate cancer] in the PSA gray zone," the group concluded.