PET/MRI scans show the progression of endometrial cancer in patients and may help predict survival outcomes, according to a study published September 13 in Academic Radiology.
Researchers led by I-Lun Shih, MD, of National Taiwan University in Taipei, found that certain imaging details on PET/MRI exams were associated with how long patients lived without disease progression. The information could be helpful for determining treatment approaches, they suggested.
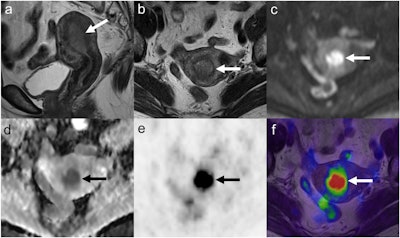
Images of a 69-year-old woman with endometrial cancer, grade 1 endometrioid adenocarcinoma, T1aN0M0, stage IA. Sagittal (a) and axial (b) T2-weighted MRI show an endometrial tumor (arrow), without deep myometrial invasion. The tumor (arrow) is hyperintense on diffusion-weighted imaging (c) and hypointense on the ADC map (d). The ADCmin of the tumor was 0.45 × 10−3 mm2/s, and the ADCmean was 0.58 × 10−3 mm2/s. PET (e) and PET/MRI fusion images (f) show intense FDG uptake of the tumor (arrow). The SUVmax of the tumor was 12.5, MTV was 3.9 mL, and TLG was 29 g.
After a median follow-up of 80 months, 15 (22%) patients had tumor progression, and six (9%) patients had died. Patients with higher metabolic tumor volume and total lesion glycolysis on the PET/MRI exams had significantly shorter rates of progression-free survival, according to the findings.
The researchers noted that patients with high MTV also had significantly shorter overall survival, with a hazard ratio of 10.84 (p = 0.033).
"This study found that PET/MRI biomarkers in patients with endometrial cancer were associated with pathological prognostic factors, disease progression, and survival," the researchers wrote.
The researchers noted that the cutoff value of metabolic tumor volume for determining prognosis in the study was 32.6 mL, but that further studies are needed to establish a standardized method for measuring metabolic tumor volume and to define the optimal cutoff value.
"This imaging biomarker might provide additional information for the risk stratification of patients," the group concluded.