A newly developed imaging method, granzyme B PET, can non-invasively detect inflammatory bowel disease (IBD) and provide a real-time picture of active inflammation in the tissue, according to new research published in the July issue of The Journal of Nuclear Medicine. Information garnered from the PET images can be used to monitor IBD treatment efficacy and could potentially guide more personalized patient management strategies in the future.
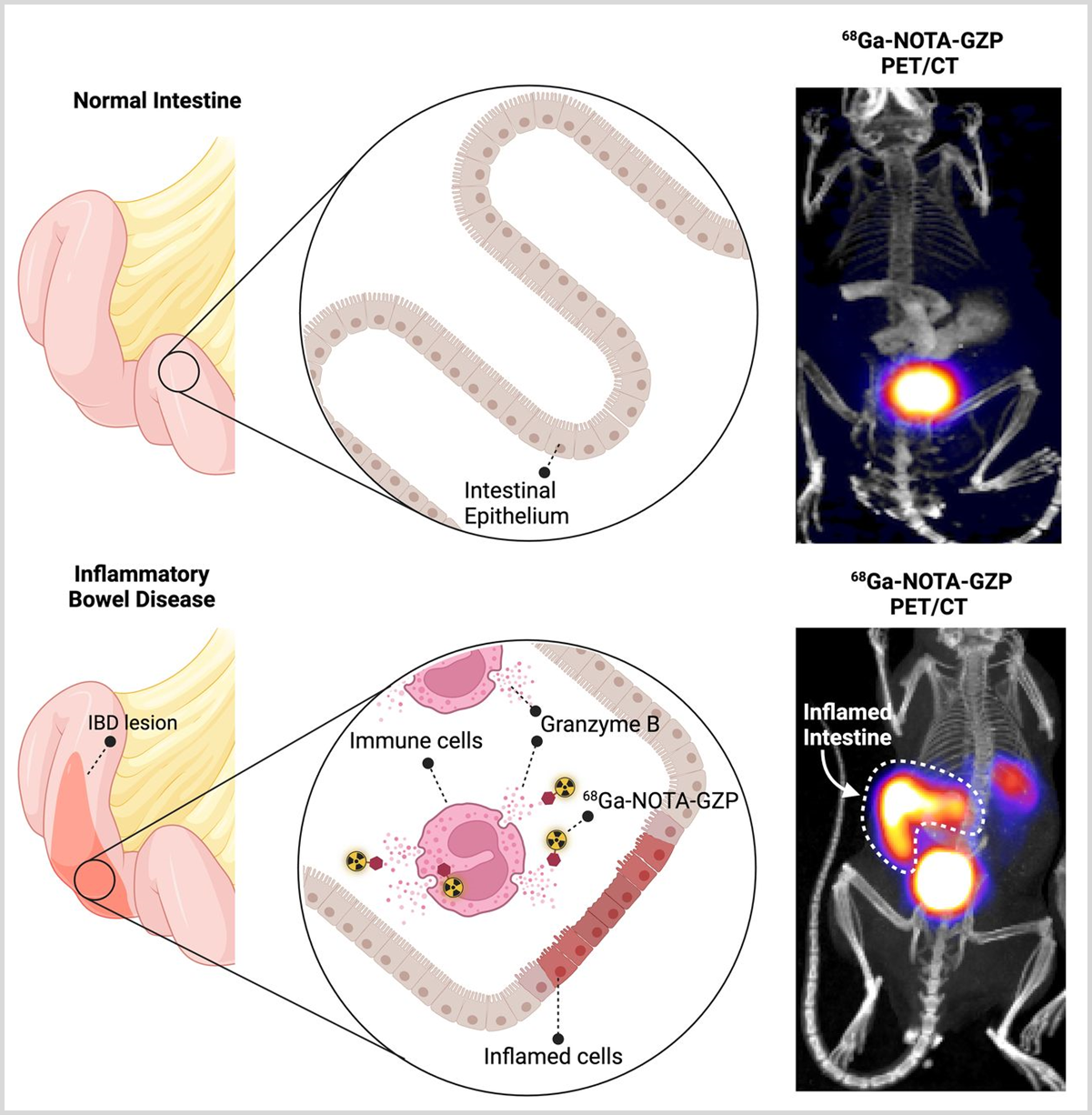
Visual Abstract. Active bowel inflammation disrupts the bowel cell lining, which causes the inflammatory T cells to secrete Granzyme B into the extracellular space, progressively accentuating the inflammatory response through a feed-forward mechanism. In the normal or non-inflamed bowel, there is no extracellular Granzyme B and therefore, 68Ga-NOTA-GZP PET does not show any uptake in the bowel (upper panel), while with active inflammation, the secreted active form of Granzyme B is detected and quantifiable by 68Ga-NOTA-GZP PET imaging (lower panel).
When the bowel is inflamed, it damages the cells lining the bowel. This damage makes certain immune cells, called T cells, release a substance called Granzyme B into the space outside the cells. This release causes more inflammation in a cycle that keeps worsening. In a healthy or non-inflamed bowel, there is no Granzyme B outside the cells, so a special imaging scan called 68Ga-NOTA-GZP PET doesn’t show anything in the bowel (as seen in the top image). However, in a bowel with active inflammation, the released Granzyme B is detected and measured by the 68Ga-NOTA-GZP scan (as seen in the bottom image).
IBD is a chronic gastrointestinal inflammatory disorder and includes two major groups: Crohn’s disease and ulcerative colitis. Although there have been notable advancements in the clinical management of IBD, substantial challenges remain in enhancing diagnostic precision, overcoming issues with treatment intolerance, and addressing the recurrent cycle of remission and relapse. In addition, long-standing IBD is associated with an increased risk of cancer, which necessitates constant monitoring of disease activity.
“Currently, there is no accurate method to detect and differentiate active inflammation from chronic disease. MRI and CT look at the structural changes in the bowel, while other imaging techniques look at the increased number of immune cells in the tissue. None of the tools, however, capture the dynamic nature of immune responses in the colon,” said Pedram Heidari, MD, radiologist and service chief of nuclear medicine at Massachusetts General Hospital, Harvard Medical School, in Boston, Massachusetts. “A non-invasive imaging method to detect immune system activation with high resolution is key to improving IBD management.”
In the study, Heidari and colleagues assessed the potential of the granzyme B gene as a biomarker for detecting IBD and predicting treatment response. Human tissue samples of Crohn’s disease and ulcerative colitis (both active and inactive disease), as well as of the noninflamed bowel, were stained to measure the expression of granzyme B. Compared to noninflamed bowel tissue, granzyme B was upregulated significantly in diseased tissues, with active disease recording higher levels of granzyme B than inactive disease. Tissue samples from IBD treatment responders and non-responders were also measured, and lower granzyme B expression was found in the responders than the non-responders.
Next, the researchers evaluated changes in granzyme B expression in a murine model including colitis-induced and control mice. Mice were imaged with 68Ga-NOTA-GZP PET at one, three, and four weeks. PET imaging showed significantly increased bowel uptake of 68Ga-NOTA-GZP in mice induced with colitis versus control mice. After treatment, 68Ga-NOTA-GZP uptake in colitis-induced mice decreased, however, the uptake in colitis-induced mice remained significantly higher than the control at all times.
“Granzyme B PET can help with the timely detection of the active disease, determination of the need to start treatment, and monitoring the response to treatment to ensure the resolution of the inflammation. This is particularly important for monitoring inflammation in the parts of the bowel that are not accessible for endoscopy and tissue sampling,” stated Heidari. “This is a unique tool that can significantly change the trajectory of disease by closely monitoring treatment efficacy and is the true definition of precision medicine.”
The authors of “Granzyme B PET Imaging for Assessment of Disease Activity in Inflammatory Bowel Disease” include Pedram Heidari, Arvin Haj-Mirzaian, Suma Prabhu, Bahar Ataeinia, Shadi A. Esfahani, and Umar Mahmood, Center for Precision Imaging and Division of Nuclear Medicine and Molecular Imaging, Department of Radiology, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts.