Targeted tumor therapy limits the therapeutic effect or drug effect to specific target cells, tissues or organs as much as possible without affecting the function of normal cells, tissues or organs thus improving the efficacy and reducing the toxic and side effects. The use of targeting molecules to direct radionuclides into tumor tissue to achieve nuclide targeted therapy is one of the important methods for tumor treatment. The main strategy of targeted therapy is to carry out radioimmunoassay or polypeptide receptor-mediated radionuclide therapy by using monoclonal antibodies or small peptides to carry therapeutic radionuclides, and specifically combine them with antigens or ligands expressed on the surface of tumor cells.
PRRT is a kind of molecular targeted radiotherapy, which uses the specific radiopharmaceuticals chelated by rapeutic nuclides (90Y, 177Lu, 111In, 131I, 225Ac, etc.) with peptides to specifically bind to the receptors rich expressed on the surface of tumor cells, with the aim of delivering cytotoxic radiation sources to tumors over-expressing specific receptors. Like cruise missiles or ballistic missiles with nuclear warheads attacking military targets, radionuclide targeted therapy refers to the use of different radionuclides that bind to specific ligands to emit different rays, thereby accurately "killing" tumor cells.
Somatostatin SST
Somatostatin receptor SSTR exists on the surface of some normal tissue cells and malignant tumor cells, such as neuroendocrine cells and lung cancer, breast cancer, lymphoma and other tumor cells. All somatostatin SSTs can bind to SSTR, exerting physiological effects, and inhibiting the growth and development and signal conversion of this tissue cell, etc., and their effect is related to the expression degree, distribution density and affinity of receptors distributed on the cell surface.
Octreotide, a synthetic somatostatin SST, has long interaction with receptors and high affinity, and its pharmacological action lasts longer than that of natural somatostatin. Radiopharmaceuticals chelated by Octreotide with radionuclide (90Y- or 177Lu-) can target neuroendocrine tumors over-expressing somatostatin receptor subtype 2(SSTR2), significantly improving the survival of patients with neuroendocrine tumors. A 12-year follow-up study reported that after peptide receptor radionuclide therapy (PRRT), 32% of patients with metastatic or inoperable neuroendocrine tumors were still alive after 12 years.
Neuroendocrine tumor
Neuroendocrine tumors are tumors that originate from neuroendocrine cells, which are a large class of cells that have neuroendocrine phenotype and can produce a variety of hormones. Neuroendocrine cells are distributed all over the body, accordingly neuroendocrine tumors can occur in any part of the body. However, the most common neuroendocrine tumors of digestive system such as stomach, intestine and pancreas account for about 2/3 of all neuroendocrine tumors. Compared with other tumors, the incidence of neuroendocrine tumors goes up more rapidly.
Treatment of metastatic neuroendocrine tumors with 177Lu-DOTATATEPRRT
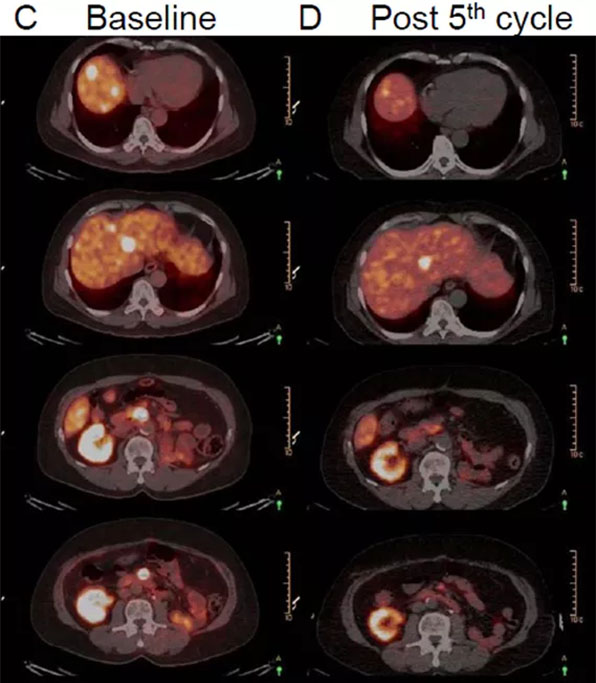
A 62-year-old male patient with mesenteric mass resection, accompanied with renal cell carcinoma of left kidney and a history of left nephrectomy. (A and C) Four years after the disease-free period, the patient experience recurrence. 68Ga-DOTATATE PET/CT showed somatostatin receptor expression and some peripancreatic nodules in IV and VIII segments. (B and D) After the fifth cycle, 68Ga-DOTATATE PET/CT showed that the lesions in the VIII segment and around the pancreas almost completely subsided, and only the lesions in the IV segment. The treatment effect was good after overall assessment.
Journal Title:
177Lu-DOTATATE PRRT in Patients withMetastatic Neuroendocrine Tumor and a Single Functioning Kidney:Tolerability and Effect on Renal Function. JOURNAL OF NUCLEAR MEDICINETECHNOLOGY • Vol. 44 • No. 2 • June 2016
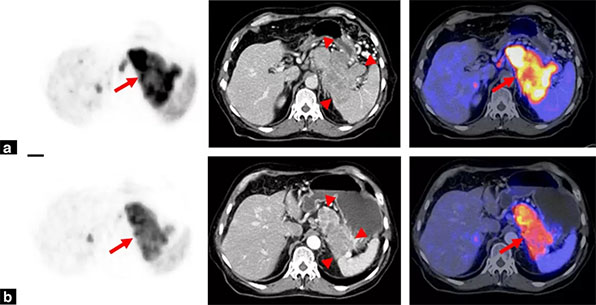
A 63-year-old male suffered from metastatic pancreatic neuroendocrine tumor (PET, CT and Fusion). (a) and (b) showed that before and after RIV treatment with 3730 MBq of 90Y-DOTATOC respectively. After treatment, 68Ga-DOTATOC tracer markers decreased (arrow), tumor volume decreased (arrow), tumor markers decreased, and the weight loss of patients improved, indicating that the treatment effect was good.
Journal Title:
Radiothérapieinterne vectorisée des tumeurs neuro-endocrines avec 90Y-DOTATOC : la fixationpréthérapeutique du 68Ga-DOTATOC est-elle prédictive de la réponse autraitement Journal de Radiologie Diagnostiqueet Interventionnelle (2014) 95,292—303
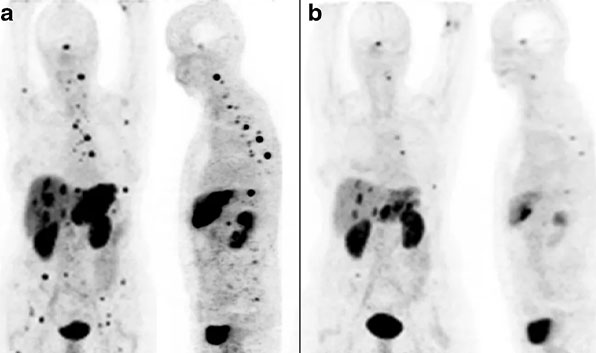
The patient had liver tumor and bone metastases. (a) showed the 68Ga-DOTATOC-PET image before treatment. After the hepatic artery injection of 213Bi-DOTATOC with 10.5 GBq, the liver metastasis was obviously reduced. After 6 months, it was observed that 213Bi-DOTATOC reached the whole body through blood circulation, which also reduced most bone marrow metastases (b)
Journal Title:
213Bi-DOTATOCreceptor-targeted alpha-radionuclide therapyinducesremission in neuroendocrinetumours refractory to betaradiation: a first-in-human experience.Eur J NuclMed Mol Imaging (2014) 41:2106–2119